How does the hyperbaric chamber trigger regeneration?
Hyperbaric oxygen therapy is a powerful therapy that can have many benefits for our health. Scientific advances on the subject are continuing and demonstrate that it would even be possible to trigger repair mechanisms at the cellular level . Which is very interesting for our body and our brain! In this article we will discover in more detail the effects of the hyperbaric chamber on our cells and what science says on this subject.
Our cells need oxygen
Did you know that oxygen is the third most abundant element in the universe, after hydrogen and helium? About 300 million years ago, the oxygen content in the air was 35%, which may have contributed to the large size of animals and insects at the time.

Photo credit: Jcomp - Freepik.com
Throughout evolution, all mammals have adapted to provide an optimal level of oxygen to the cells of their body. In humans, the oxygen distribution chain begins in the lungs and ends in the mitochondria of our cells.
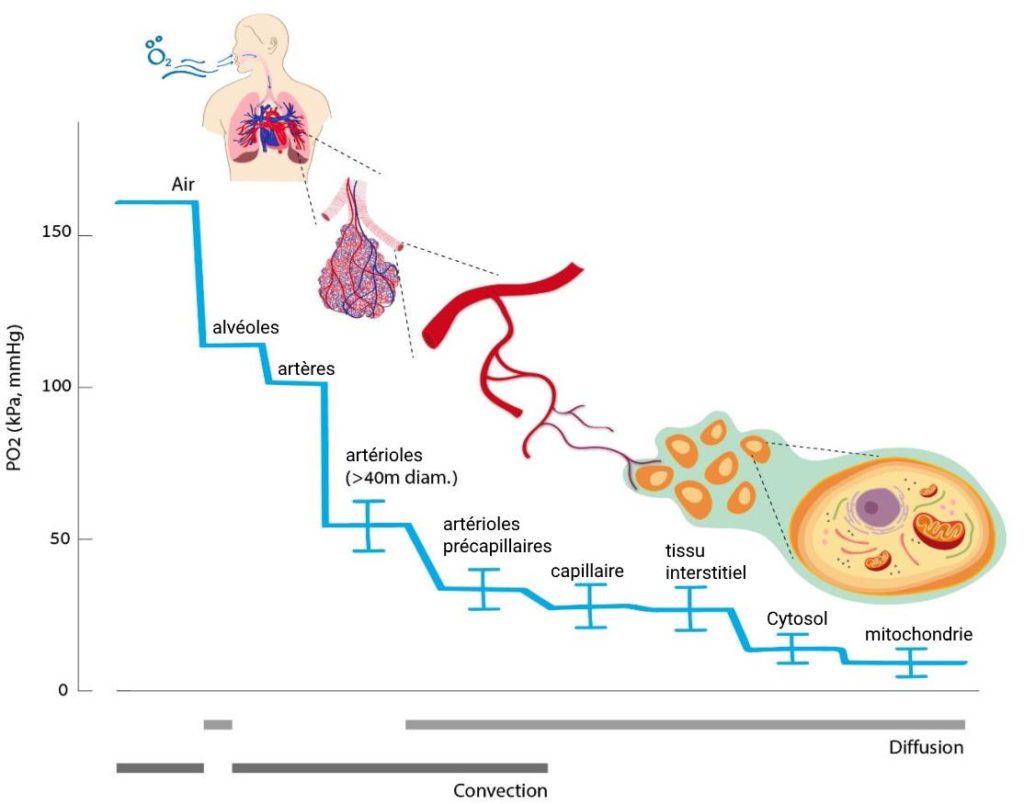
Credit: Biomolecules. 2020 Jun, doi: 10.3390/biom10060958
These little powerhouses use 80% of the oxygen we breathe, as well as the food we eat, to produce energy (ATP). This is called cellular respiration.
Cellular oxygen demand can vary depending on the needs. For example, an exercising muscle has a higher oxygen demand than a resting muscle. Therefore, there are several mechanisms and reflexes that allow the human body to maintain an adequate oxygen supply. Among them, increased ventilation and dilation of the pulmonary arteries
Our ability to maintain a constant supply of oxygen is essential to the proper functioning of our cells... and to our survival! But what happens when our cells are deprived of oxygen?
The cellular response to hypoxia
The fundamental importance of oxygen has been known for centuries, but the discovery of how the body adapts to its availability only dates back to 1938.
Hypoxia-inducible factor (HIF)
Warning: Before continuing to read this article, keep in mind that the goal is to popularize and make the information accessible to all. If you have advanced knowledge in biology, I invite you to directly consult the scientific sources available at the end of the article.
Depending on the availability of oxygen, a protein complex called HIF-1α is found in greater or lesser quantities inside our cells:
- At normal oxygen levels, HIF-1α proteins are degraded by a cellular process called the proteasome.
- When oxygen levels are low, our body has fewer reactive oxygen species ( ROS ) to break down this HIF-1α complex. As a result, its quantity increases and the alarm bells go off! HIF-1α ends up activating certain genes encoded in our DNA.
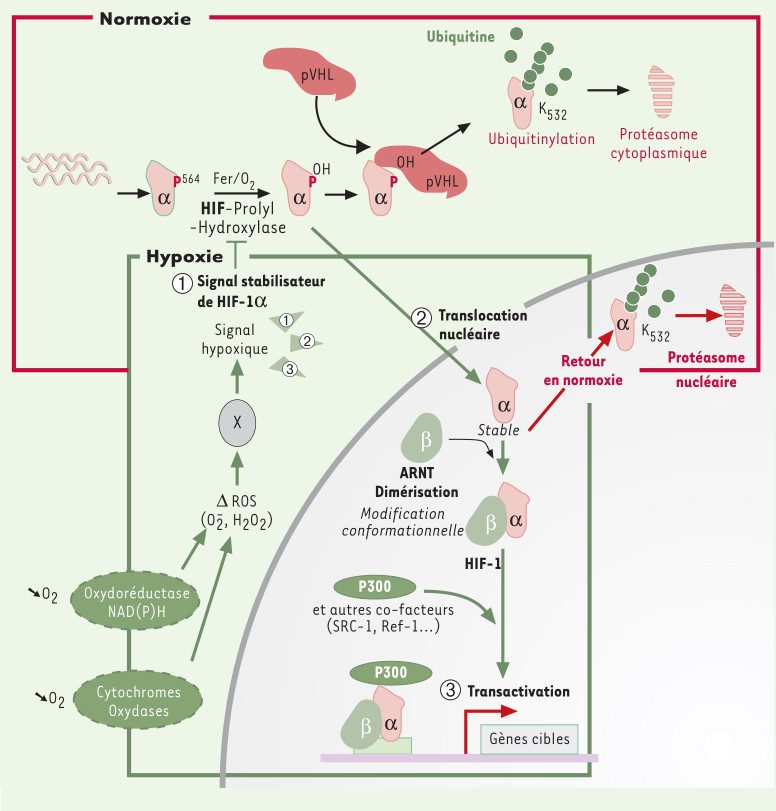
Proteins that activate genes are called transcription factors.
HIF is the true conductor of the cellular response to hypoxia
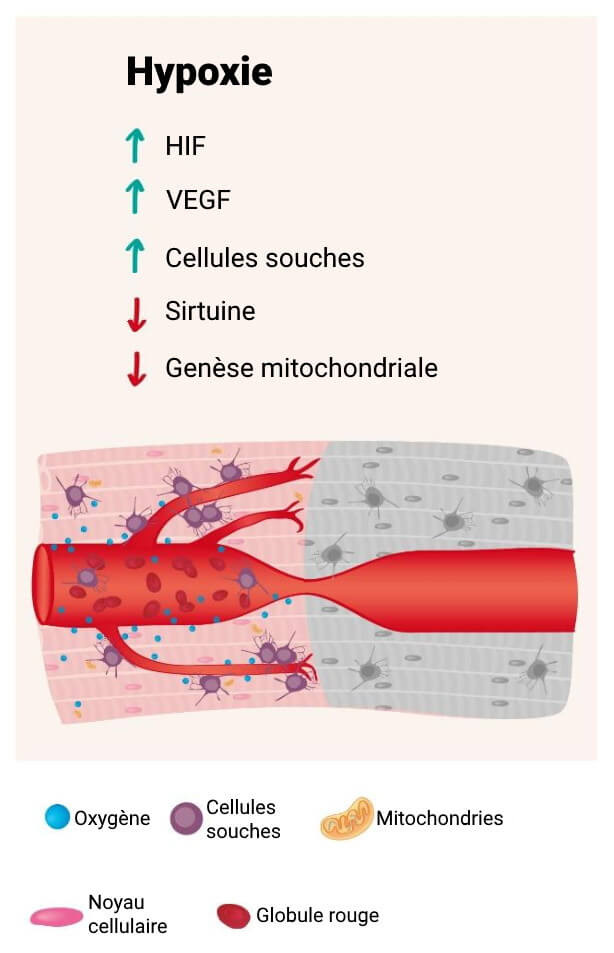
In addition to stimulating many genes, the hypoxia-induced factor triggers important regeneration processes in our body:
- Vascular endothelial growth factor (VEGF), which allows the formation of new vessels from a pre-existing network. This is called angiogenesis
https://pubmed.ncbi.nlm.nih.gov/18504100/ . - Proliferation and migration of stem cells
https://pubmed.ncbi.nlm.nih.gov/19698058/ .
However, prolonged hypoxia also brings its share of negative effects at the cellular level:
- A decrease in mitochondrial biogenesis and the number of mitochondria
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6453877/ . - Our sirtuins are also downregulated. Sirtuins are enzymes that regulate a wide range of biological processes, from gene transcription to energy metabolism
https://www.frontiersin.org/articles/10.3389/fphys.2021.752117/full .
So, as you can see, hypoxia is the natural trigger of important metabolic processes. Positive (triggered by HIF ), but also negative (triggered by the lack of O2!).
The Hypoxic Hyperoxic Paradox
And now, what if I told you that it is possible to trick our cells? Using a hyperbaric chamber , it is possible to activate this famous HIF , but without being in a state of hypoxia...
We saw a little above that our cells have the ability to detect prolonged hypoxia. And fortunately for us, this ability is fallible! Indeed, the cells would interpret the following 2 situations in the same way:
- To move from a state where oxygen is available to a state where it is lacking.
- Moving from a state where our body is over-oxygenated in a hyperbaric chamber (hyperoxia), to a normal state (normoxia).
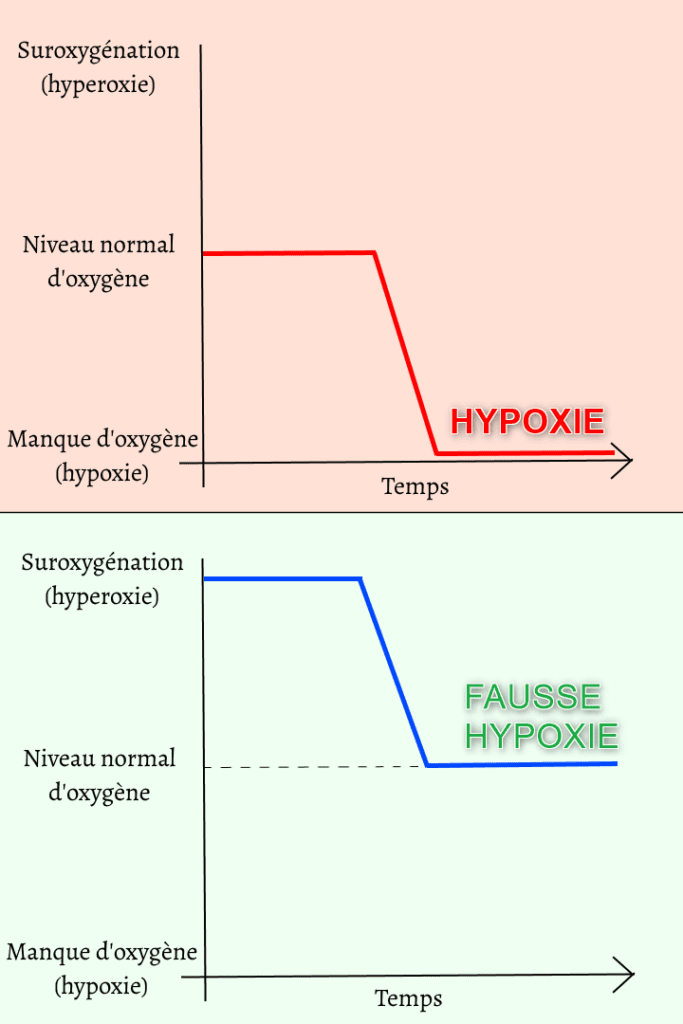
Thus, moving from hyperoxia to normoxia would activate HIF and trigger the cascade of regeneration processes. All while avoiding hypoxia !
This is called the hypoxic-hyperoxic paradox.
The effects of the hypoxic hyperoxic paradox on our cells
Researchers explain the effects of the hypoxic-hyperoxic paradox on our cells using the following hypothesis:
- Under normoxic conditions, oxygen and reactive oxygen species are available. HIF-1α degradation therefore occurs.
- During hyperoxia in a hyperbaric chamber, oxygen availability is increased, which naturally enhances our production of reactive oxygen species and antioxidants.
- Upon return to normoxia after a single hyperoxic exposure, the ratio of reactive oxygen species to antioxidants will be elevated.
- Upon return to normoxia following repeated hyperoxic exposures, the ratio of reactive oxygen species to antioxidants will be low. This is similar to a hypoxic state! HIF-α protein degradation therefore does not take place and the alarm signal ( HIF ) is then triggered!
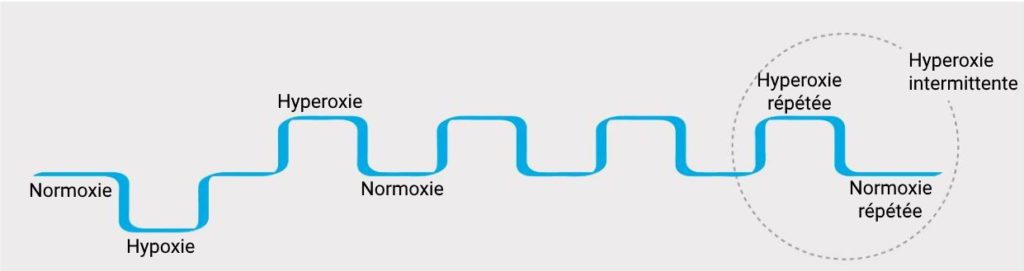
This means that intermittent and repeated hyperoxia in a hyperbaric chamber simulates hypoxia by unbalancing the ratio between reactive oxygen species and antioxidants.
What are the effects of the hyperbaric chamber on our cells?
The beneficial effects of the hypoxic-hyperoxic paradox are multiple. Here are some examples from the scientific literature:
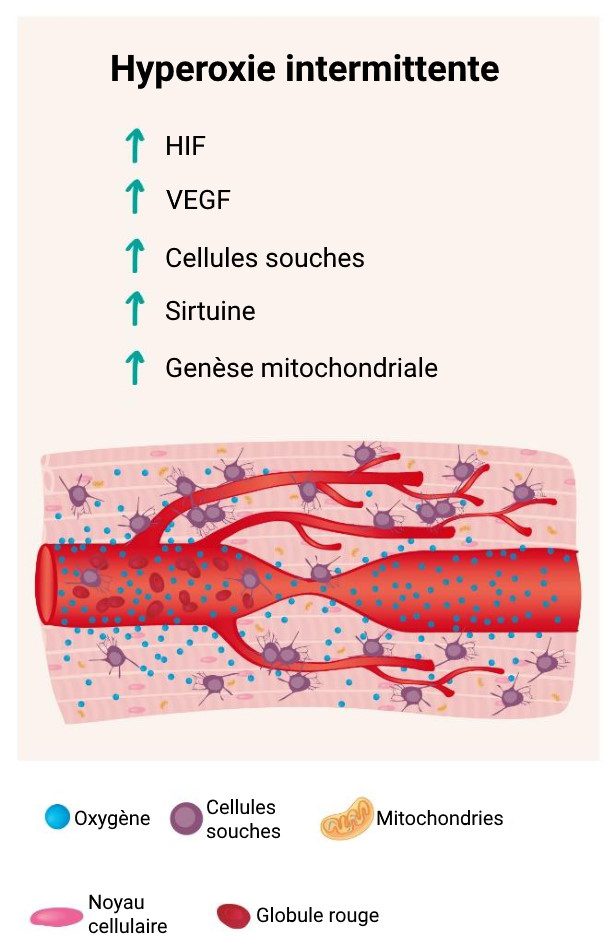
-
HIF : The effect of repeated intermittent hyperoxia in a hyperbaric chamber has been demonstrated on different types of organs and cells. For example, on damaged brain cells
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4102647 , of the digestive systemhttps://www.ncbi.nlm.nih.gov/pmc/articles/PMC5021505/ and liverhttps://pubmed.ncbi.nlm.nih.gov/18644387/ . -
VEGF : Angiogenesis is stimulated after intermittent hyperoxic exposures. Hyperbaric oxygen therapy can initiate cellular and vascular repair mechanisms to induce cerebral angiogenesis and improve blood flow in damaged brain regions
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5654341/ . -
Stem cells : Intermittent hypoxia and hyperoxia stimulate stem cell proliferation. Studies in brain-injured patients have shown that repeated sessions in a hyperbaric chamber increase the number of circulating stem cells, and this correlates with observed clinical improvements.
https://pubmed.ncbi.nlm.nih.gov/28779582/ . -
Sirtuin : Intermittent hyperoxic exposures stimulate the activity of sirtuins. Sirtuins have a neuroprotective effect that has been studied in several animal models. Sirtuins lead to attenuation of cerebral infarction and improve neurological function
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5489129/ . -
Mitochondria : Hyperbaric oxygen therapy allows much more oxygen to be delivered to the mitochondria. As a result, this therapy induces the biogenesis and migration of mitochondria, which helps maintain neuronal function.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4084443 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4968589 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6630002 .
Now you know why hyperbaric chamber sessions are regenerative!
Conclusion
Many advances have been made in recent years regarding hyperbaric oxygen therapy. Observing the progress and improvements that benefit patients is an important thing. But we also absolutely must decipher all the cellular mechanisms in order to understand why this therapy is regenerative. Each new scientific study on this subject is a step closer to the use and democratization of this therapy to treat the brain.
