Treating a brain using a hyperbaric chamber

Professor Shai Efrati currently heads one of the largest hyperbaric oxygen therapy centers in the world: The Sagol Center .
He launched a research program focused on the biological effects of hyperbaric oxygen therapy and more particularly on cerebral neuroplasticity (regeneration of damaged brain tissue).
In this video, he explains to us very simply how and why it works.
The rest of the article is a transcription of this video.
Shai Efrati explains how to heal a brain using hyperbaric oxygen therapy
Hello everyone, I am very happy to be here. Before we start talking about our new therapeutic approach, we must first understand what we are treating... And that is why we should look at the target.
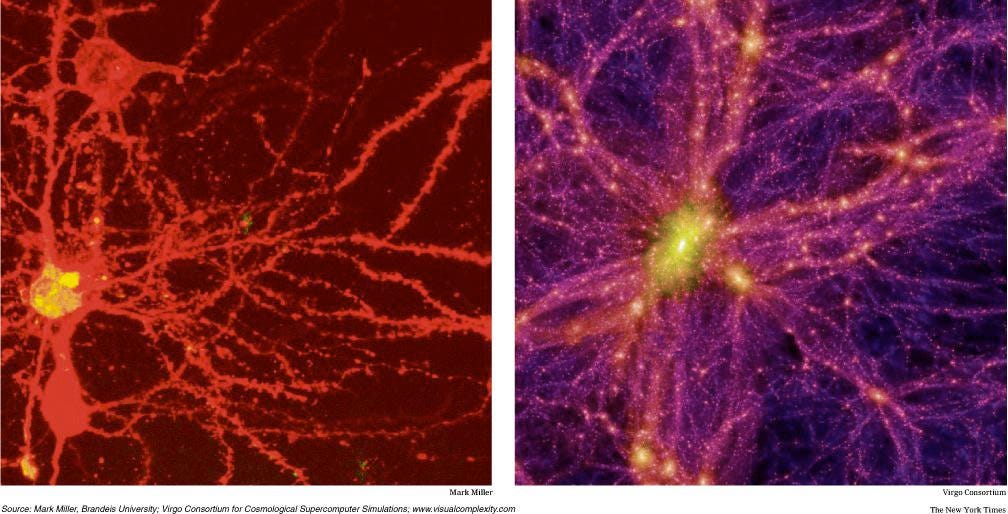
You can see on the right side the universe. It's big. It's actually huge. It's going to be very difficult for us to understand, all the different ingredients and all the different connections that we have in this big universe.
On the left we see the brain. A neuronal cell. And looking at it, we can say that it is huge.
It is difficult to understand all the interactions between the different elements of this system.
The main question, for me as a physicist, when I want to do something that applies to the patient. How can we simplify such a complex biological system. And in order to simplify things, we can look at this. And I'm sorry for the pictures:
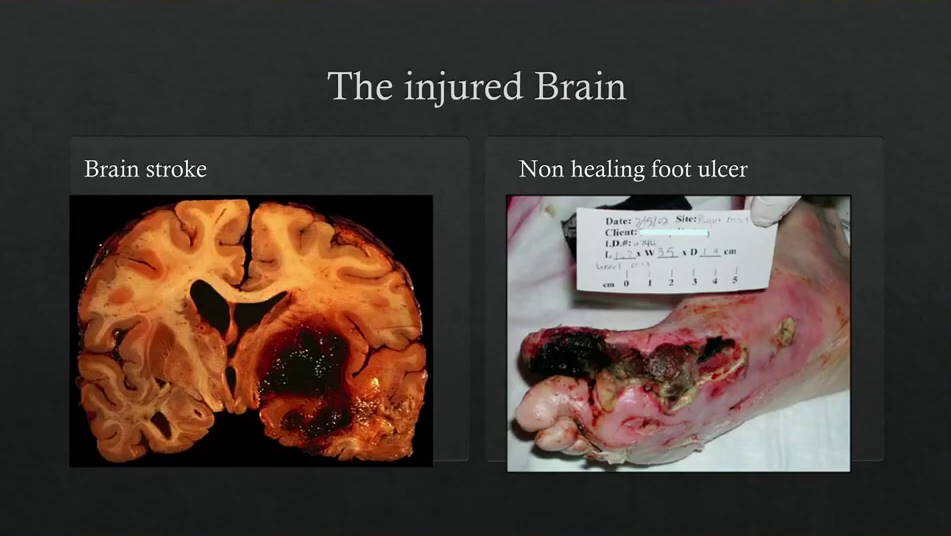
On the right, what do we see? It's the same thing. On the right, we see a classic injury. An injury that we all know. If we look at the deformed part of the foot, we can see necrotic tissue. Totally lost tissue. We can't heal this tissue. It will fall off. But close to it, we can see damaged tissue. But not completely dead. And if we bring good oxygenation and stem cells, this tissue could heal.
On the left, what do we see? It's the same thing. We see a wound and in the center of the wound, we see necrotic tissue that is totally lost. And surrounding this necrotic tissue, we see tissue that, if we provide good oxygenation and stem cells, this tissue can heal.
What is the main difference between the two? The main difference is that the leg injury, we see it, we understand what we are dealing with. But the injury here is necessary (editor's note: shows his head), it is high technology. We look at the scanner, we look at the MRI. We talk about the brain as something mystical. Cognitive... memory... personality... It is a tissue!
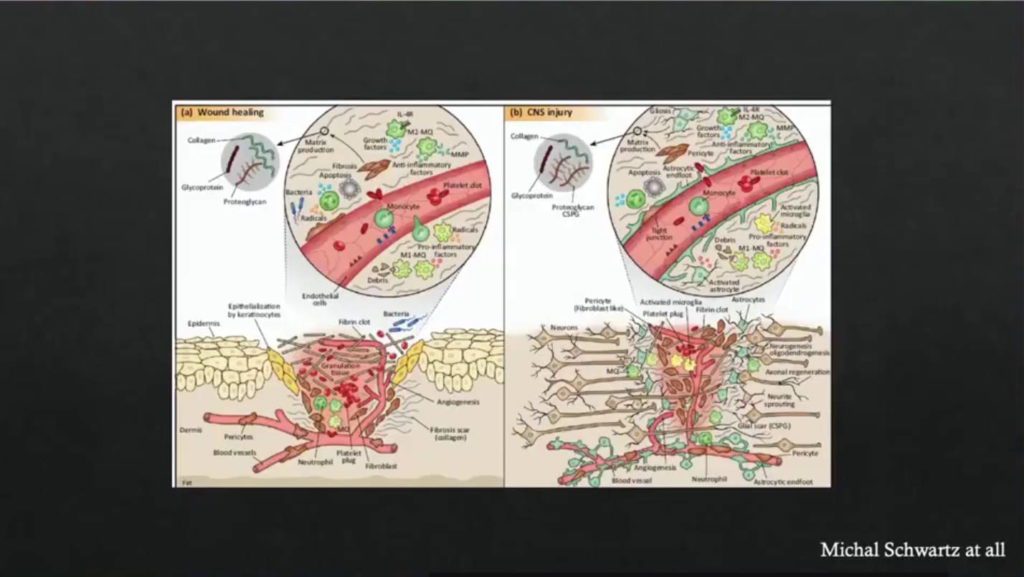
And today it is quite clear to us that the basic things that are needed to repair, to heal a peripheral wound, are the same basic things that we need to heal the wounds that we have up here (editor's note: shows his head).
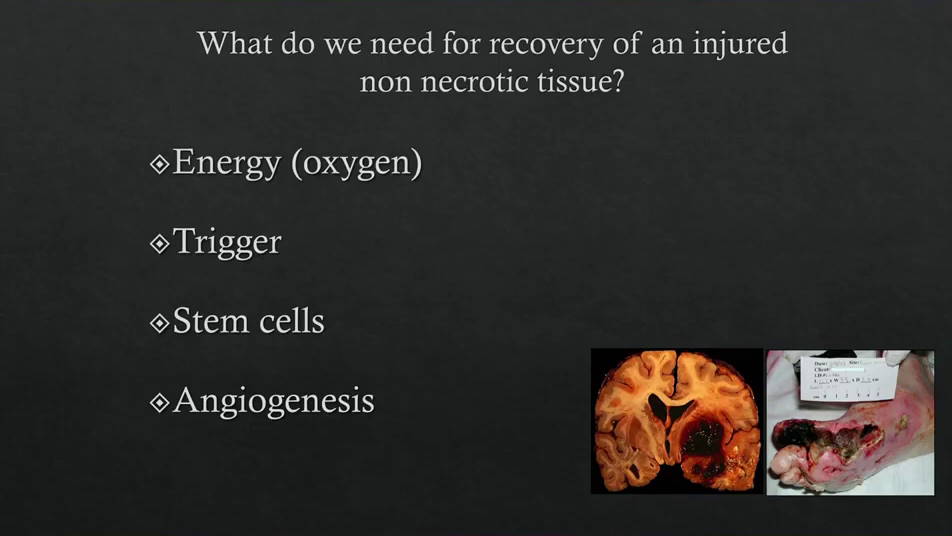
The four main things we need, as a basis for any healing process.
- Including energy because of course if we don't have enough oxygen in the tissues nothing will happen.
- We need a trigger . For any regeneration process, we need a trigger to start it.
- We need stem cells .
- And we need angiogenesis , generation of new blood vessels.
And I'll say a few words about each.
Oxygen (energy)
As far as the brain is concerned, it is 2% of our body but it consumes more than 20% of the total oxygen demand of the whole body. At any given moment, the brain uses all the oxygen that is supplied to it. And all the brain has to do is make a preference. Where should the oxygen go now, which part is most important at the moment. So if I move my hand, the perfusion will go more to the part that is responsible for the motor movement of the hand. If it is the leg, it will be the part of the leg. You can see the perfusion by MRI.
We all know this, in our routines. When I drive and I phone at the same time. I miss the turn. It is a physiological limitation. Why do I miss the turn? Because now the perfusion is mainly transferred to the part that is responsible for the discussion and less for driving, so I will miss the turn. In order to understand if oxygen is indeed a limiting factor, for the brain activity of a healthy human being, we use this: our hyperbaric center. This is what it looks like:


It's quite different from what you might think. We can put patients in there and play with pressure and gases. That's my playground. I like it. We put neurophysiology students in there, who are considered very intelligent, and we asked them to multitask. To do a motor function, at the same time as a cognitive function. It's not easy to do at the same time. We asked them to do that in "normal" conditions and also under hyperbaric oxygen.
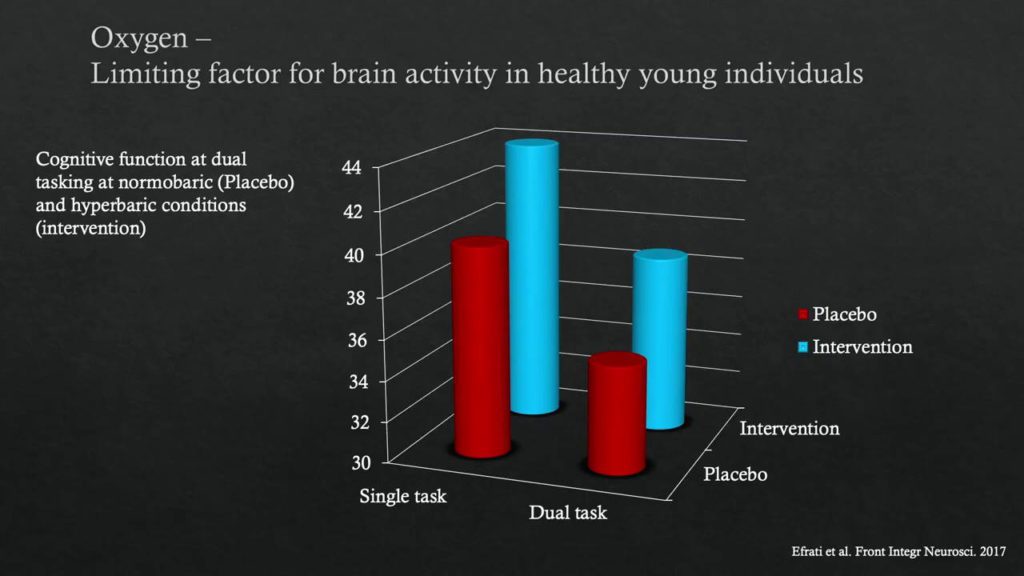
We can clearly see that even in a healthy, healthy, functioning brain, when we increase the amount of oxygen (editor's note: in hyperbaric conditions) our ability to perform a more complex task is significantly improved. Needless to say, what happens when we have brain pathology. So we have our first building block.
Hypoxia (the trigger)
The next one is: "the trigger". If you want to initiate something, we have to trigger it. And the most powerful trigger in our body, for the regeneration process, is hypoxia. Hypoxia has been in the news in the last two weeks, because there are 3 Nobel Prize winners regarding the cascade of factors induced by hypoxia.
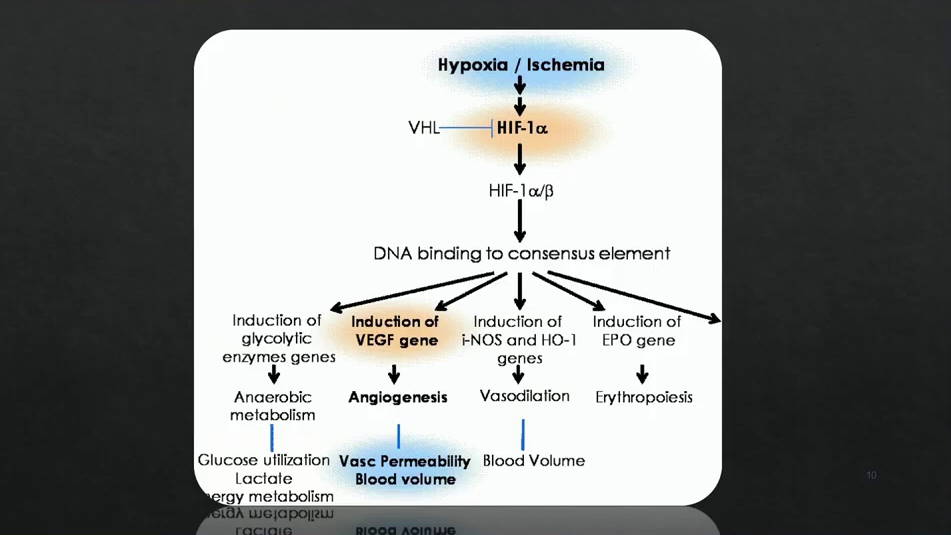
When we have hypoxia, HIF (Hypoxia-Inducible Factor) increases.
HIF is a transcription factor and when it is activated, many genes, downstream of the cascade, will be regulators. Among others, we have for example VEGF (Vascular Endothelial Growth Factor). We will have new blood vessels that will be generated. It turns out that the body does not actually feel the absolute value of oxygen. The body feels the fluctuation at the cellular level.
Because hypoxia is dangerous, we put the patient in the hyperbaric chamber, we increase the oxygen to a very high level, and then we decrease it rapidly by asking them to take their mask off and then put it back on. By doing this fluctuation, the body senses this decline (hyperoxia to normoxia) as hypoxia. And so we induce HIF. We call this the hyperoxic-hypoxic paradox. At the cellular level, we can see that when we do this, the cell responds by increasing HIF.
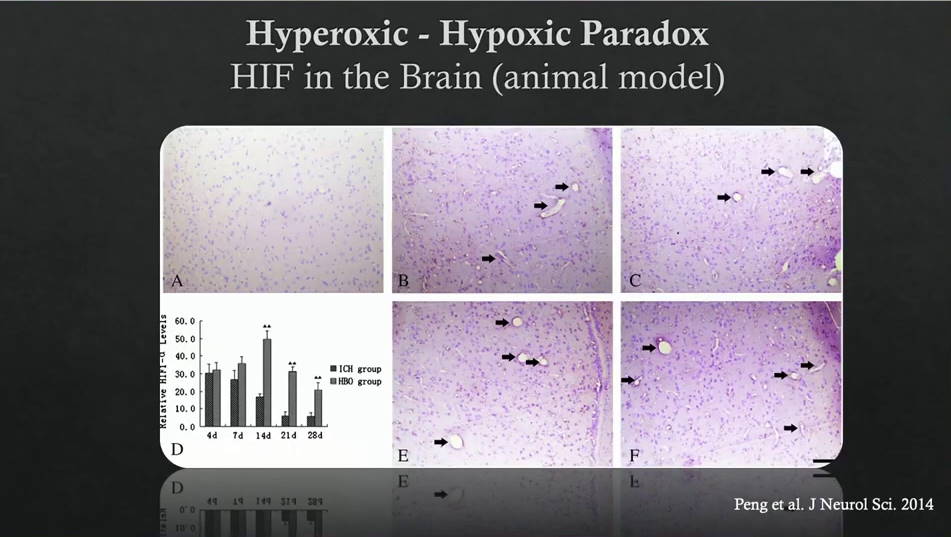
We can also see it at the tissue level, in this rat brain we can see the induction of HIF.
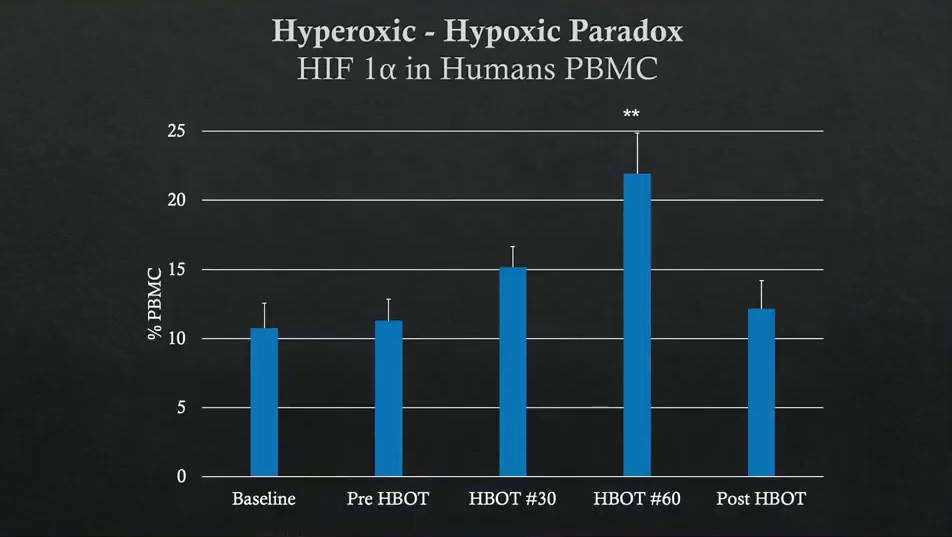
We also see this in humans, with repeatable treatment. After 30 sessions and 60 sessions, the external environment is perceived as hypoxia even though we are not in hypoxia. So we have HIF.
Stem cells
Another thing we need is stem cells. I don't need to explain stem cells to you, I play with them a lot in our lab. We thought about taking stem cells to the next level. Instead of extracting them and injecting them. To stimulate the body, to produce stem cells. How do you do that? Again, with the fluctuation! High oxygen, then a rapid decline back to normal. By doing this, you can see the dramatic increase in hematopoietic stem cells, which we measure in a blood sample.
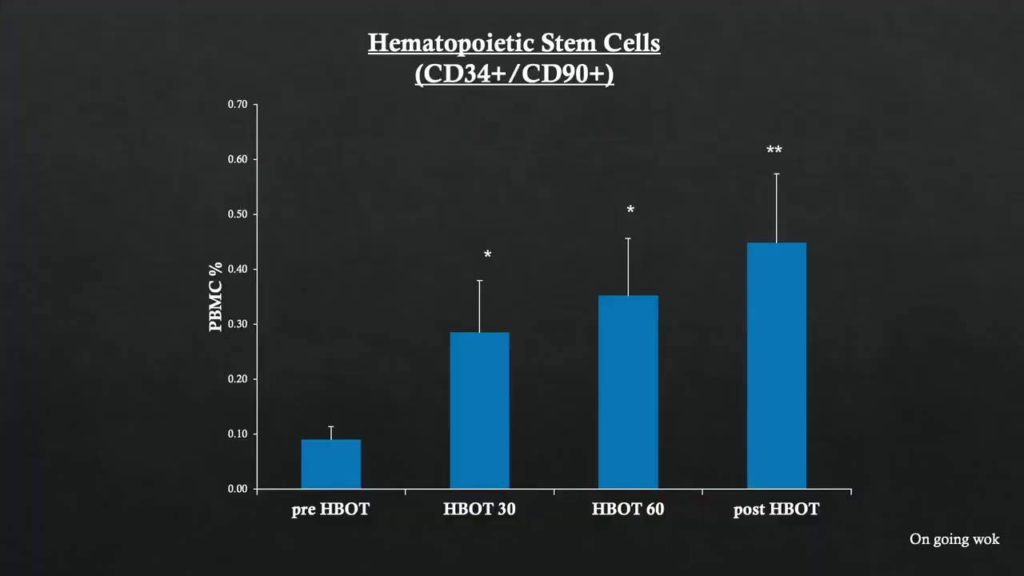
And the most exciting thing is, for the first time, we see that we can also trigger the proliferation of mesenchymal stem cells in humans.
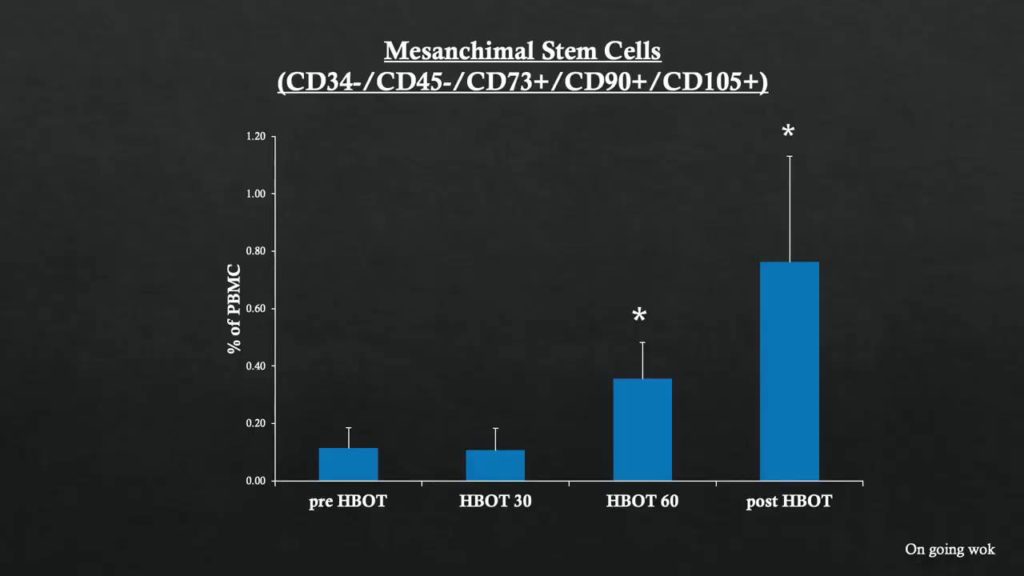
Mesenchymal stem cells are the cells that we have in the tissue. We can make them proliferate to the point where we can detect them in the blood.

What happens if we take the best plant in the world, and plant it in the desert in the picture on the left? Probably not much, it will die. But if we take that plant and put it in good soil with enough water, it will grow and proliferate. So it's not enough to just take the stem cells, especially if we're dealing with damaged tissue.
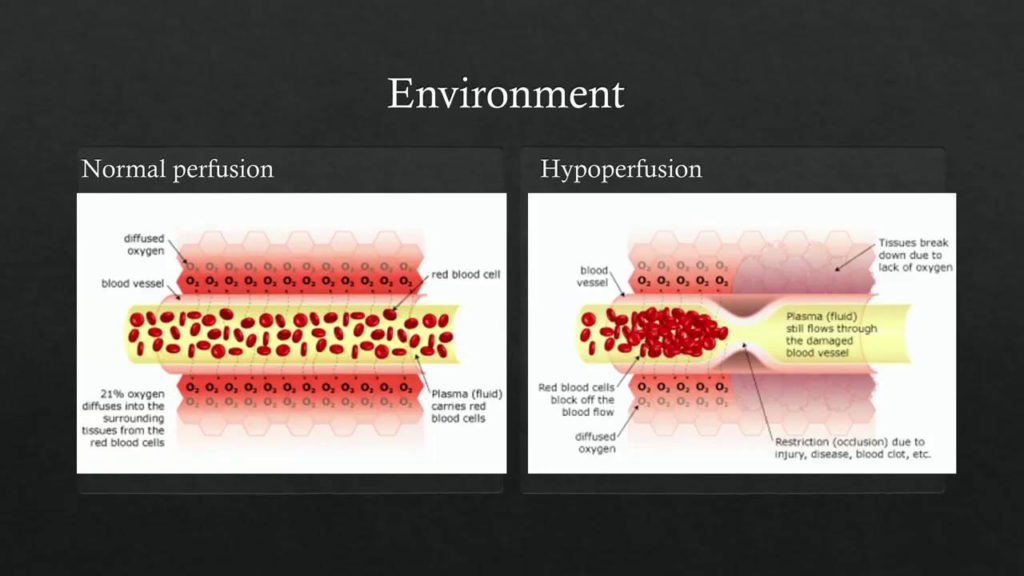
On the left you can see tissue with normal perfusion. This is not damaged tissue.
We have damage in a relatively hypoperfused tissue (editor's note: on the right), where we don't have enough oxygen. We don't have enough water for the plants. In this case, if you put the stem cells here, it will be very difficult for them to grow.

By placing this tissue in a hyperbaric oxygen environment, we can increase the dissolved oxygen in the blood to such a level that we no longer need red blood cells. Once we go above 2 atmospheres, the amount of dissolved oxygen in the blood is sufficient for all the energy demand. Thus, blood (oxygen) will diffuse even to poorly perfused damaged tissue.
Angiogenesis
That's good, but if we want to do something persistent we need angiogenesis.
And for angiogenesis we will need stem cells, a trigger and energy. So we have everything!
And indeed, we can clearly see the angiogenesis being generated.
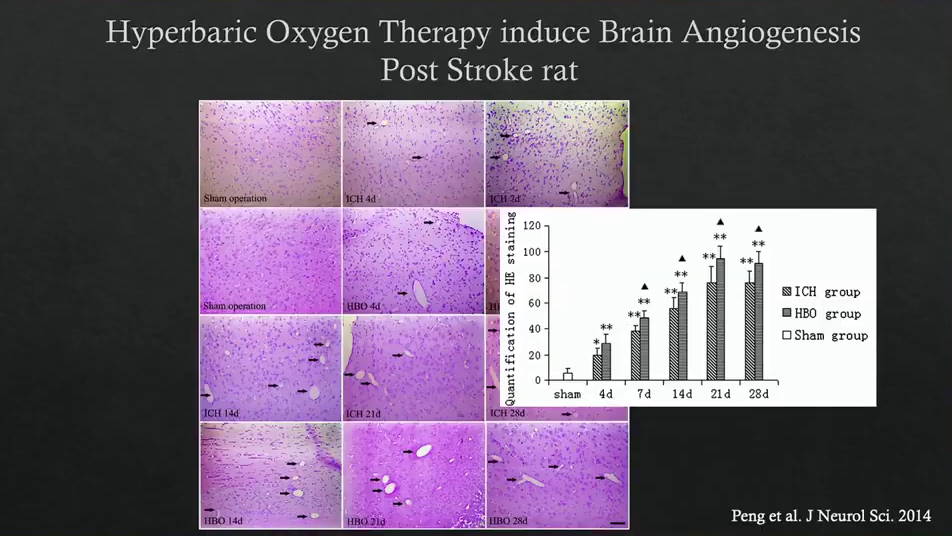
This is a special stroke rat (editor's note: a breed of laboratory rat specially modified to have a stroke).
We can see it even more beautiful, as you can see here in our normally aging rat colony.
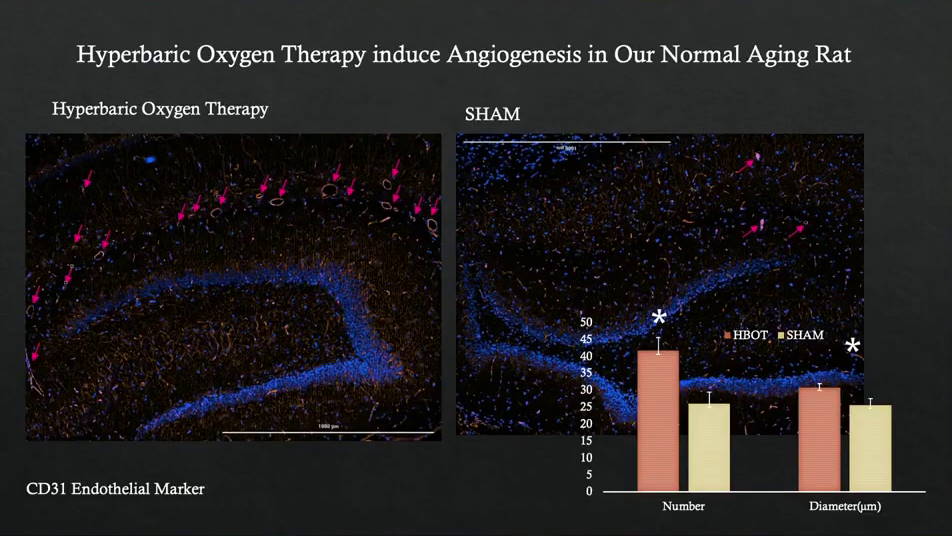
We have a colony of aging rats in our lab and we can see that by inducing hyperbaric… not hyperbaric… it's the fluctuation that we generate with oxygen. We can stimulate angiogenesis in the brain.
It can also be seen in humans, using perfusion MRI:
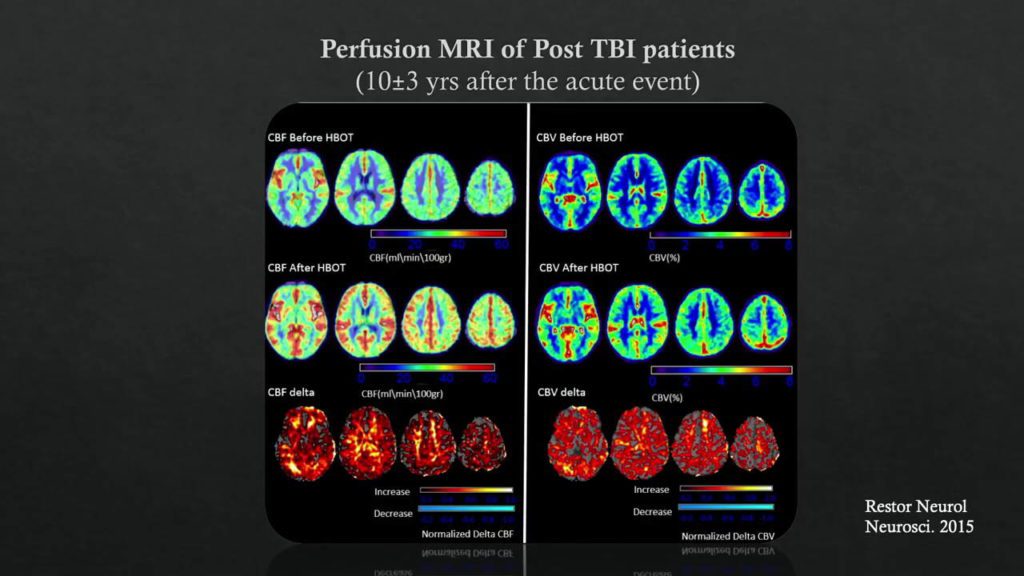
We can see the change, in cerebral blood flow and cerebral blood volume. And that means we can actually generate angiogenesis in the human brain.
Brain imaging
So now we have everything: the energy, the trigger, the stem cells and the angiogenesis.
So the next important question is: what is the optimal wound? How do we select the optimal wound that will be suitable for this treatment? To do this, we need good brain imaging.
We need imaging that combines anatomical and metabolic imaging of the brain. And that's what we're doing here. We're combining SPECT with MRI, while making it simple for physicists. We're not very smart, especially the one in front of you. I need it to be simple. And we use colors:
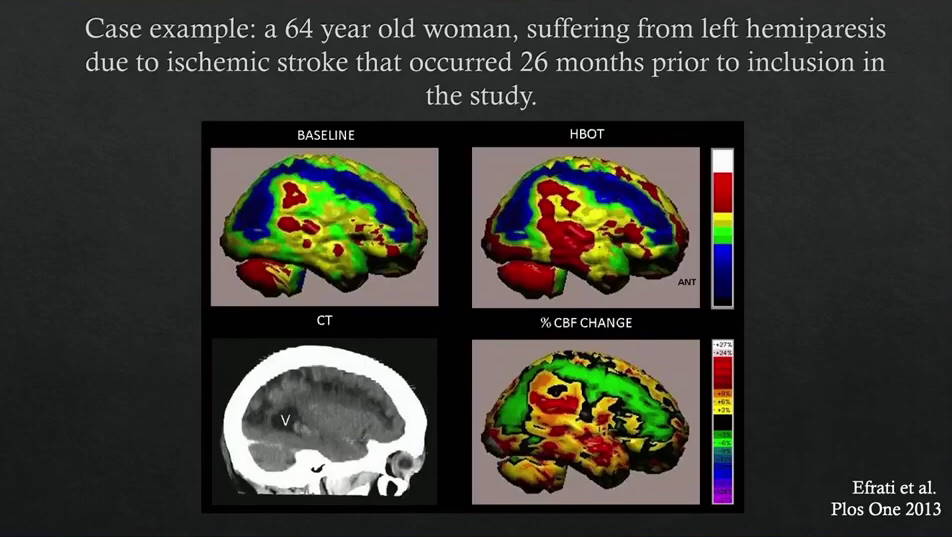
- In blue we mark the necrotic area, which is completely dead.
- Green is metabolic dysfunction.
- Red is the fully functional fabric.
You can clearly see that blue remains blue, what is necrotic remains necrotic. But green, metabolic dysfunctional tissue can be rejuvenated and regenerated.
The clinical presentation will follow the part that has been healed. So if it is the part responsible for the hand, the hand will move. If it is the part responsible for the leg, the leg will move.
And the important thing is that you can predict the outcome with the patient. You can say, "I don't think your leg is going to move, but I think you're going to talk again." "Is that okay with you? Yes or no?"
He can say yes or no. If he says yes, his wife can refuse: "I don't want him to talk!" That's another problem. It's very exciting to see and to discuss with the patient. But that's our job.
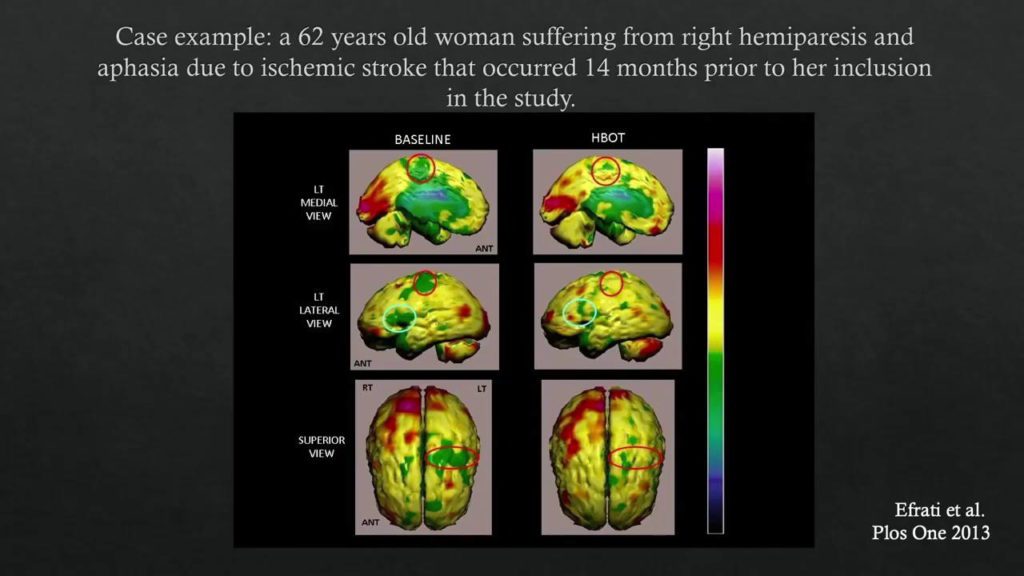
Here's another classic example: a stroke victim who can't move his hand and leg. And look at the top line on the left, the dysfunctional metabolic tissue that's responsible for the hand and leg. The green has turned yellow. That means the hand and leg are moving again.
On the second line, you see Broca's area in green. She (the patient) cannot speak. And after treatment, she can speak. We were not treating her ability to speak. We are only treating injuries. And no matter who is responsible for this injury, it will happen. Our job is to treat these injuries. It does not matter where the injury is.
We can see other examples:
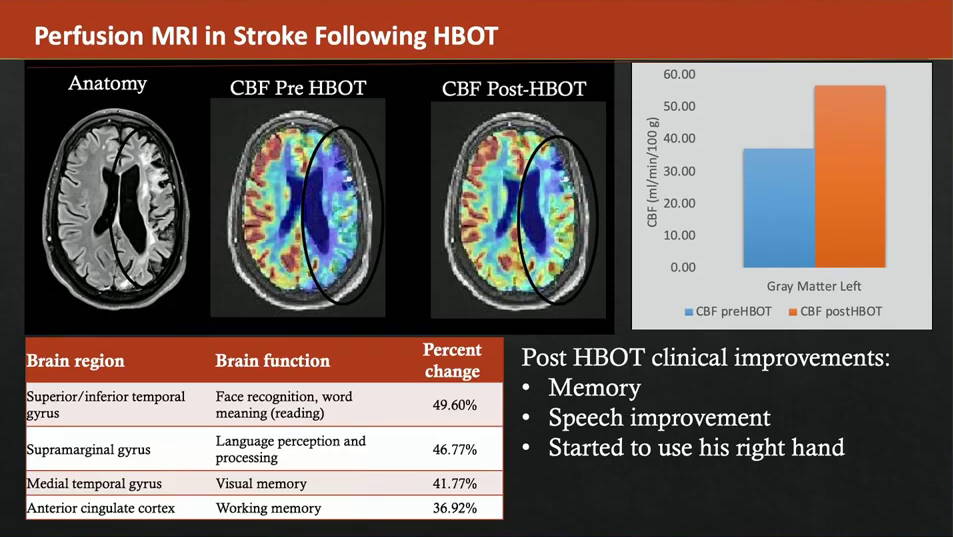
Today we use perfusion MRI and DTI and this is another example. You can see the "classic" anatomical MRI on the left. You can see the perfusion of the MRI, combined with the anatomical imaging.
You can see the before and after and see how cognitive function has improved dramatically. Again, we're not treating cognitive function, we're treating injuries.
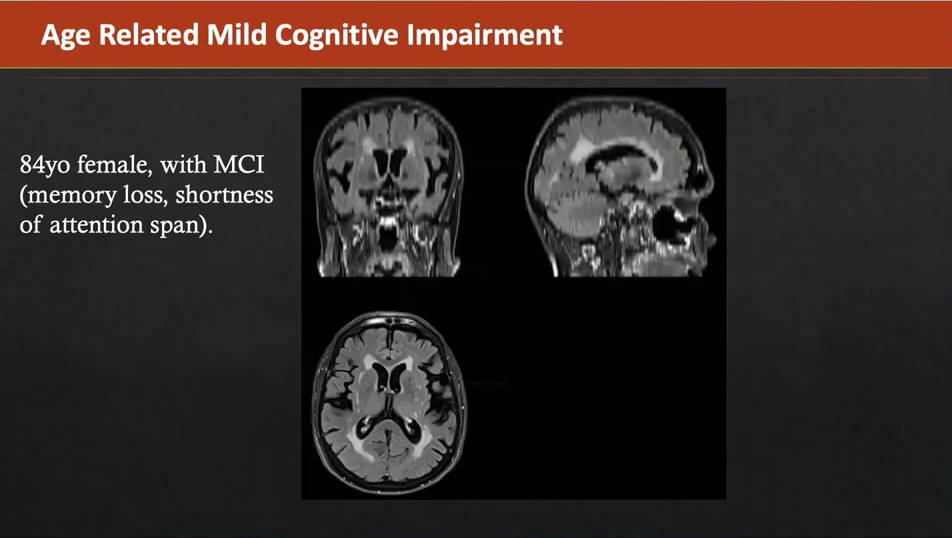
We have a project going on, what's called age-related cognitive decline. That's a topic for another conference, maybe next year. What we see in age-related cognitive decline, we see the white spots in the brain on the MRI and that mark is a gimmick lesion in the brain. It's medium perfusion, small tissues and this patient is perfectly healthy. She hasn't had a stroke, she hasn't had a heart attack, she hasn't had diabetes. Just age-related cognitive decline.
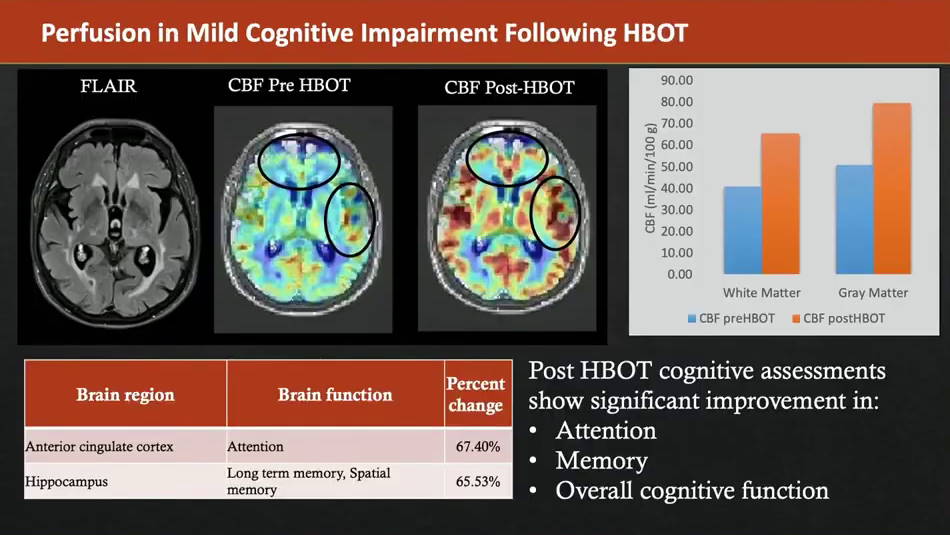
And again, we are in the wound domain. We see a proper wound, we treat the wound! In the middle you can see the "before" and on the right "the after". You can see the significant increase in perfusion. No discussion. This is your brain before, this is your brain after. We can measure the Delta. Of course, the cognitive functional units improve but we do not treat the cognitive. We treat the wounds.
Conclusion
I'm going to pause here because my time is up, but what we're presenting here is a new perspective on how to look at the brain as a tissue! Surprise, surprise! It is indeed a tissue and the basics that are needed to heal injuries to limbs or other parts of the body, the basics are also needed for injuries that we have inside for this tissue that we see indirectly. All we need to do is present the brain in the same way that we see other injuries in the body. Thank you very much.
How does a session in a hyperbaric chamber take place?
Below, I offer you a short video to show you concretely the progress of a session (which is also called " diving ") in a hyperbaric chamber. Subtitles are available for the hearing impaired.
